Pregnancy in women with history of ischemic stroke and thrombophilia
Makatsariya A.D., Akinshina S.V., Bitsadze V.O., Zhuravleva E.V., Idrisova L.E., Abramyan G.R. Дата публикации на сайте: 2015-09-21 Доступна также в печатной версии журнала Резюме | Полный текст | Скачать в PDF
Резюме:
Currently due to reduction of direct causes of maternal mortality increasing interest of scientists cause arterial thrombotic complications. Pregnancy-related stroke is a rare event, however, when it occurs, may be life threatening and there may be implications for management of the patient and delivery. The mechanisms and risk factors for ischemic stroke related to pregnancy and in women of childbearing age remain unclear. Pathogenesis of so severe complication in young women is not fully understood, however, there is a concept thrombosis or cerebral embolism, which can develop on the background of well-known population-based risk factors such as hypertension, metabolic syndrome, smoking, heart rhythm disorders, valvular heart disease or in relation to typical obstetric pathologies, such as preeclampsia, massive obstetrical bleeding, septic complications, amniotic fluid embolism. In recent years, there is increasing interest in the role of thrombophilia in the pathogenesis of ischemic stroke, however, data on this issue is even more limited and contradictory than for venous thrombosis. Methods of prevention of recurrent stroke and strategies of pregnancy and delivery management in women with history of ischemic stroke are also contradictory.
DOI: 10.17749/2070-4968.2015.9.2.089-098
Received: 05.05.2015; in the revised form: 30.05.2015; accepted: 22.06.2015.
Conflict of interests
The authors declared that they do not have anything to disclosure regarding funding or conflict of interests with respect to this manuscript.
All authors contributed equally to this article.
For citation
Makatsariya A.D., Akinshina S.V., Bitsadze V.O., Zhuravleva E.V., Idrisova L.E., Abramyan G.R. pregnancy in women with history of ischemic stroke and thrombophilia. Akusherstvo, ginekologiya i reproduktsiya / Obstetrics, gynecology and reproduction. 2015; 2: 89-98.
Corresponding author
Address: ul. Zemlyanoi Val, 62-1, Moscow, Russia, 109004.
E-mail address: gemostasis@mail.ru (Makatsariya A.D.).
БЕРЕМЕННОСТЬ У ЖЕНЩИН С ИШЕМИЧЕСКИМ ИНСУЛЬТОМ И ТРОМБОФИЛИЕЙ В АНАМНЕЗЕ
Макацария А.Д., Акиньшиина С.В., Бицадзе В.О., Журавлева, Идрисова Л.Э., Абрамян Г.Р.
ГБОУ ВПО «Первый МГМУ имени И.М. Сеченова» Минздрава России, Москва
Резюме
В настоящее время в связи с уменьшением числа непосредственных причин материнской смертности повышенный интерес у ученых вызывают такие осложнения, как артериальные тромбы. Беременность редко является причиной инсульта, тем не менее, если он имеет место, то может представлять собой угрозу жизни и повлечь за собой осложнения в процессе ведения пациентки и родов. Механизмы и факторы риска при ишемическом инсульте, вызванном беременностью, и у женщин детородного возраста остаются неясными. Патогенез такого серьезного осложнения у молодых женщин полностью не изучен, тем не менее, имеет место концепция о вероятном развитии тромбоза или церебральной эмболии на фоне общеизвестных популяционных факторов риска, таких как гипертония, метаболический синдром, курение, нарушения сердечного ритма, порок сердца или в связи с такими типичными родовыми патологиями как преэклампсия, обширное кровотечение при родах, септические осложнения, амниотическая эмболия. В последние годы возрастает интерес к роли тромбофилии в патогенезе ишемического инсульта, тем не менее, данные, имеющиеся по этому вопросу, носят даже более ограниченный и противоречивый характер, чем по венозному тромбозу. Также противоречивы способы профилактики повторного инсульта и стратегии ведения беременности и родов у женщин, имеющих в анамнезе ишемический инсульт.
Kлючевые слова:
Ишемический инсульт, беременность, тромбофилия, антифосфолипидный синдром, низкомолекулярный гепарин.
Статья поступила: 05.05.2015 г.; в доработанном виде: 30.05.2015 г.; принята к печати: 22.06.2015 г.
Конфликт интересов
Авторы заявляют об отсутствии необходимости раскрытия финансовой поддержки или конфликта интересов в отношении данной публикации.
Все авторы сделали эквивалентный вклад в подготовку публикации.
Для цитирования
Макацария А.Д., Акиньшина С.В., Бицадзе В.О., Журавлева Е.В., Идрисова Л.Э., Абрамян Г.Р. Беременность у женщин с ишемическим инсультом и тромбофилией в анамнезе. Акушерство, гинекология и репродукция. 2015; 2: 89-98.
Ключевые слова: Ишемический инсульт, беременность, тромбофилия, антифосфолипидный синдром, низкомолекулярный гепарин.
First Moscow State Medical Sechenov University of the Ministry of Health Russian Federation
Concepts of traditional risk factors of ischemic insult
Epidemiologic data signify that in people younger than 35 the risk of stroke is higher in women compared to men, while women suffer from more severe consequences of the complication, including the risk of lethal outcome and disability [13,45]. Stroke during pregnancy is a rather rare event and is developed based on different data with frequency from 4.2 to 210 per 100,000 childbirths, however it is considered very grave complication where the lethality may reach 8-26% [7,49]. Approximately 12 to 35% cases of stroke in people aged 15 to 45 years are related to pregnancy [22,23]. Pregnancy is even called “spontaneous screening test for the risk of early stroke” [4]. In pregnancy there is noted the increase of stroke risk by 3-13 times [20], however, due to the limited number of studies dedicated to the issue, and enrollment of small number of patients, the precise statistic analysis is very difficult. A number of authors state approximately equal increase of risk of hemorrhagic and ischemic strokes related to the pregnancy [49]. In majority of cases (to 90%) stroke develops in III trimester of pregnancy and in postnatal period [45]. Based on the data of study by Kittner SJ (1996) risk of ischemic stroke in postnatal period increases 5-fold compared to the non-pregnant patients of the same age (HR 5.4, 95% CI 2.9-10.0), and the risk of hemorrhagic stroke increases 18-fold (HR 18.2, 95% CI 8.7-38.1) [22]. It is worth to note that the risk of stroke stays increased during rather long period of time after childbirth [44,49]. Tang C.H. et al. (2009) upon analyzing 139 hemorrhagic and 107 ischemic pregnancy-related strokes, have established that the relative risk of such complications in patients with preeclampsia is respectively 10.7 and 40.9 during III trimester of pregnancy, 6.5 and 34.7 during 3 days post childbirth, 5.6 and 11.2 from 3 days to 6 weeks postpartum, 11.8 and 11.6 from 6 weeks to 6 months postpartum and 19.9 and 4.3 from 6 to 12 months postpartum [44]. It is possible that the reason for increased risk of stroke in postnatal period is the change in hemostasis system towards hypercoagulation, intended for protection against blood loss in birth, as well as abrupt decrease in circulating blood volume, fluctuations of hormonal level and changes in the structure of vessel walls. The data indicate the necessity for long follow-up, control of hemostasis system condition and development of rehabilitation methods in this group of patients.
Factors for the stroke development risk in pregnancy include the same reasons as the ones for non-pregnant women: arterial hypertension, atherosclerosis, smoking, heart valves diseases, prosthetic heart valves, atrial fibrillation, migraine, systemic lupus erythematosis, systemic vasculites. The reasons for ischemic stroke may include thromboses, embolisms, spasm of brain vessels, hypoperfusion. However, while in elderly people the main cause of stroke is atherothrombosis, which frequently associates with a lot of underlying long-term chronic conditions, including arterial hypertension, dyslipidemia, diabetes mellitus, ischemic heart diseases, only 15-25% of pregnant women with fatal stroke were found to have atherosclerotic damage of vessels [50]. Moreover, in women of childbearing age the stroke frequently develops in completely healthy state without preceding clear risk factors [40]. At the same time a number of pregnancy complications (severe forms of gestational toxicosis, amniotic fluid embolism, obstetric hemorrhages, postnatal septic complications) are the entirely separate, specifically stroke-provoking factors. The data signify the necessity for detailed study of stroke risk factors in women of childbearing age and the fact that many of those factors are still unknown.
Special group of risk for development of arterial thromboembolisms in pregnancy is the patients with heart valve disease: expressed, hemodynamically significant prolapse of mitral valve with high degree of regurgitation, rheumatic heart diseases, prosthetic heart valves. For example, in bacterial endocarditis the frequency of cerebral thromboembolism reaches 20% [50]. Risk of thromboembolism significantly increases in the heart rhythm disorders, most frequent one of them being the atrial fibrillation. For example, the risk of arterial thromboembolism development in atrial fibrillation is 10-23%, while brain thromboembolism risk is 5-10%.
Presence of open foramen ovale (OFO), which with development of ultrasound diagnostics becomes detectable in general population in up to 30% of cases, is a well established risk factor of cryptogenic stroke in young people and is detected in such patients in approximately 50% of cases. In conditions of heart rhythm disorder the risk of cardioembolic stroke in OFO increases even more [40]. Taking into account hypercoagulation typical for normal gestation process and possible changes of hemodynamic parameters in childbirth which may lead to inversion of pressure gradient and facilitation of right to left shunting, the risk of cardioembolism in patients with OFO can be even higher, especially in case of thrombophilia present. In the rare cases paradoxical embolism may be caused by amniotic fluid embolism.
There is noted the increase of the stroke development risk in pluripara women, in cesarean section compared to the unassisted birth, also, the risk of stroke increases significantly with the age of pregnant woman (from 30 cases per 100 thousands at the age younger than 20 to 90.5 per 100 thousands in the age older than 40). Cesarean section based on the data by different authors is associated with increased stroke risk by 3-12 times [12,20], which cannot be ignored due to the continuing tendency of towards increasing the number of indications for cesarean section and appearance of the term of “cesarean section at request of patient”.
The risk of both ischemic and hemorrhagic stroke increases in the patients with severe forms of gestational toxicosis. 25-45% of patients with pregnancy related stroke had preeclampsia or eclampsia [45]. Moreover women with the pregnancy complicated by gestational toxicosis has 60% higher risk of development of ischemic stroke not related to pregnancy, and family history of development of cardiovascular diseases and in particular stroke is a risk factor for development of gestational toxicosis [32]. It is interesting that metabolic syndrome is an underlying process for development of both cardiovascular complications and the typical pregnancy complication namely gestational toxicosis. Moreover, the women with metabolic syndrome, preeclampsia and placental insufficiency in anamnesis, including the fetal growth retardation syndrome, in subsequent life display increased risk of cardiovascular complications and its earlier development [35]. All of this signifies the originally existing genetic or acquired factor, predisposing to development of both obstetric and cardiovascular complications with thrombophilia being one of such factors.
New data on pathogenesis of ischemic stroke
Pathogenesis of stroke development in gestational toxicosis conditions so far remains unknown. A number of mechanisms is proposed including the formation of endothelial dysfunction which makes gestational toxicoses related to atherosclerosis, disorder of autoregulation of brain vessels and increase of perfusion pressure leading to barotraumas and damage of vessels, hemoconcentration, activation of coagulation cascade and inflammatory response with development of DIC-syndrome and formation of microthrombosis and multiorgan failure [36]. It is worth to note that thrombocytopenia which is stated by the researchers to be the risk factor for stroke in pregnancy, may be a manifestation of APS, HELLP-syndrome, DIC-syndrome, with noted activation of platelets, development of hyperaggregation conditions, platelets consumption and formation of prothrombotic potential [20].
Recently the increasing attention was paid to the issue of relation between hormonal therapy and stroke risk, in particular in use of hormonal contraception, replacement hormonal therapy (RHT), assisted reproductive technologies. Risk of stroke in use of OC increases in average by 3 times [29]. A number of authors report the relation between the mutation of prothrombin G20210A and mutation of FV Leiden and ischemic stroke in young people. Pezzini A. et al. (2007) in the study involving 108 women with ischemic stroke using OC showed that the risk of stroke with use of OC in absence of thrombophilia increases by 2.65 times (95% CI 1.46-4.81), and in presence of minimum of one of studied thrombophilia factors (FV Leiden, mutation of prothrombin G20210A, MTHFR С677Т) – almost by 23 times, which is much higher that the result presumed during summing up certain values of stroke risk related to OC intake or thrombophilia, at the same time, taking into account upper border of 95% confidence interval, relative risk in such women may increase to 116! [34].
Interesting data were received when analyzing the outcome of over one million childbirths in Sweden. The risk factors for venous thromboembolisms and stroke in this population were preeclampsia, end of the third trimester of pregnancy, childbirth and postnatal period, cesarean section, large number of childbirth in anamnesis. At the same time the risk of vascular complications increased by 3-12 times [37]. However the statistical analysis showed that those well known risk factors cannot completely explain increased risk of vascular complications during the pregnancy requiring search of other hidden causes of gestational venous and arterial thromboses.
Since Rudolf Virchow discovering in 1884 the three main factors for thrombi development (slowed down blood flow, damage of wall of vessel, changes of the blood properties) a number of mechanisms predisposing to thromboses was established and found, however even with clear analysis of all the risk factors the cause of thromboses in 50% of cases remains unknown (the so-called “idiopathic” thromboses) [33]. Pregnancy in itself is a condition where the risk of venous thromboses development increases by 5-6 times [41]. Actually, all the signs of Virchow triad are typical for physiological pregnancy. During the pregnancy we can observe progressive increase in content of procoagulant factors, decreased activity of anticoagulant system due to development of resistance to activated protein С (АРС), slowdown of fibrinolysis.
In the recent years the increasing attention is paid to the study of the role of thrombophilia conditions, both for development of obstetric complications and for development of thromboembolic complications. In general population genetic forms of thrombophilia (FV Leiden mutation, prothrombin mutation, С and S proteins deficiency, antithrombin III) and antiphospholipid syndrome (APS) (acquired thrombophilia) on average happen in 15-20% of population, and in venous thromboses based on the literature data the frequency of thrombophilias reaches 50% [10]. In a number of thrombophilia conditions the risk of VTE increases by over 100 times, especially in the presence of homozygous, multigenic forms of thrombophilia or combined forms (genetic thrombophilias + APS) [41].
Resistance to activated protein С happens on average in 3%-7% among European population and in 20%-30% of patients with thromboses [39]. Classic example of APC resistance is FV Leiden mutation, during which factor V and VIII became insensitive to inactivating effect of protein С, which leads to excess thrombin formation and fibrinolysis slowdown. APC resistance also may happen in other mutations of V factor (FV Hong-Kong, FV Cambridge, HRII-haplotype), as well as entire number of acquired factors including APLA circulation, treatment with oral contraceptives (OC), infections, obstetric complications against the chronic DIC-syndrome, mostly in conditions of gestational toxicosis.
Mutation of prothrombin G20210A is associated with increased level of prothrombin (activity of factor II reaches 130% and more) and is detected in 2-5% of healthy population. In this mutation the VTE risk increases on average by 3 times [21]. Mutation of prothrombin G20210A was detected in 17% of pregnant patients with VTE.
The studies of the recent years signify clear relation for genetic thrombophilias and APS with such pregnancy complications as fetal loss syndrome, fetoplacental insufficiency (FPI), fetal growth retardation syndrome (FGRS), intrauterine fetal death, premature detachment of a normally situated placenta (PDNSP), severe forms of gestational toxicosis [27,31]. While previously the role of thrombophilia in pathogenesis of pregnancy complications was viewed only from the point of view of microthrombosis of placental bed vessels, presently the understanding of pathogenetic effects of thrombophilia has increased significantly. It is related to the study of the hemostasis system role and non-thrombotic effects of thrombophilia as soon as the implantation of gestation sac and invasion of trophoblast.
APS is one of the most important risk factors for thromboembolic complications during the pregnancy. Currently APS means the complex of symptoms combining clinical signs and laboratory data – presence of antiphospholipid antibodies in combination with arterial and/or venous thromboses and/or obstetric complications [21,27,31] (scheme 1). During the pregnancy thromboses manifest in 30% of patients with APS. Risk of VTE recurrence in APS is significantly higher than in general population and reaches 70%.
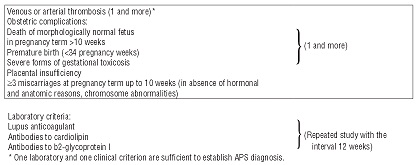 | Scheme 1. Modern criteria of aniphospholipid syndrome. |
Pathogenetic mechanisms of thromboses development in APS are the following: interaction with phospholipids for endothelial cells and platelets, prostacyclin secretion disorders, disrupted contact fibrinolysis activation, inhibition of tissue plasmonogen activator (t-PA), of thrombomodulin/protein С/protein S, induction of resistance to APC.
Hyperhomocysteinemia is related to the early development of atherosclerosis and increased risk of thromboses. The most frequent cause of hyperhomocysteinemia is mutation of methylenetetrahydrofolate reductase MTHFR С677T, frequency of which in general population is 10-20% [19]. However the literature data regarding the role of mutation MTHFR C677T as a factor for increased risk of VTE and obstetric complications are contradictory [15,28]. Hyperhomocysteinemia is the only hereditary hemostasis abnormality which is relatively easily compensated with the use of folic acid and group B vitamins. Typical for our country is the lack of concept of “healthy lifestyle” and deficiency of the necessary vitamins and antioxidants in a diet. Thus further study of the role of hyperhomocysteinemia for development of arterial thromboses during the pregnancy seems to be very important.
A number of studies studied relations between FV Leiden mutation, prothrombin G20210A mutation, defects of anticoagulant system, in particular deficiency of antithrombin III, protein C and protein S, and arterial thromboses. Results of those studies are rather contradictory and in general signify the lack of relation between those forms of thrombophilia and myocardial infarction or ischemic stroke in general population [2]. Nevertheless, the hypothesis that the thrombophilic conditions, including FV Leiden mutation and prothrombin mutation G202010А are more frequent in young patients with idiopathic stroke and myocardial infarction in young age who do not suffer from atherosclerosis were confirmed in the literature sources worldwide [17].
It was proven that hyperhomocysteinemia and MTHFR C677T mutation are the independent risk factors for arterial thromboses, including ischemic stroke, and a powerful prognostic factor of fatal outcome [17]. There was detected the association between increased level of homocystein in blood and increased risk of myocardial infarction in young women. Voetsch B. et al. (2000) detected the relation between MTHFR C677T mutation and ischemic stroke in separate ethnic groups, thus the highly important role in evaluation of relating between genetic predisposition towards hyperhomocysteinemia and the risk of arterial thromboses belongs to the specifics of national particularities of the diet and prevalence of genetic defects of folate cycle components in different populations [47].
Relation with arterial thromboses was also detected for certain defects of fibrinolysis, while the information on this issue is very limited and the topic remains the subject of continuing research and discussion.
Highly important for the patients with thrombophilias can be the exposure to additional risk factors. For example, in smoking patients with presence of FV Leiden mutation the risks of myocardial infarction and ischemic stroke increase from borderline values to 8-32-fold [25]. Martinelli I. et al. (2006) have established 2-fold increase of ischemic stroke risk during first 6-18 months of use of OC and 3.5-fold increase in patients with hyperhomocysteinemia, and with simultaneous use of OC and presence of FV Leiden mutation or hyperhomocysteinemia the stroke risk increased respectively 13-fold and 9-fold [29].
Testing for thrombophilias is necessary for the patients from younger age group with ischemic stroke which may affect the tactics of future management and development of prevention of repeated arterial and venous thrombotic complications [17]. Also there are the hypotheses that thrombophilia may affect the severity of ischemic damage, leading to more extensive thrombosis in acute phase, and cause the increased risk of recurrence [17]. Moreover, some authors state that the type of thrombophilia may determine the type of stroke manifestation. Szolnoki Z. (2001) have determined that polymorphism of ACE I/D gene is associated with microvascular infarctions, while FV Leiden mutation may lead to predisposition towards major focal brain damages [43].
A number of scientists studied the relation between thrombophilia and pregnancy-related strokes. Witlin A.G. et al. (2000), upon summarizing 20 years of work experience, have described 20 cases of pregnancy-related strokes, with one of the risk factors in such patients being genetic thrombophilia, mostly related to defects of anticoagulation system: deficiency of protein С, protein S or antithrombin III [49]. Kupferminc M.J. et al. (2000) in 12 female patients with first episode of brain ischemia during pregnancy detected thrombophilia in 83% compared to 17% in control group. The spectrum of thrombophilias studied included: FV Leiden mutation, prothrombin MTHRF С677Е mutation, deficiency of antithrombin III, protein С, protein S. Authors made the conclusion of necessity of tests for genetic forms of thrombophilia in patients with ischemic type brain circulation disorders during pregnancy [24].
Much more unambiguous data were accumulated regarding relation between the risk of arterial thromboses, including recurrent ones, and APS [3], in particular, between APS and ischemic stroke in young women. Similarly to genetic forms of thrombophilia APLA is more frequently detected in younger patients, in recurrent thromboses, in patients who have no widely known risk factors i.e. atherosclerosis detected. The stroke on average develops 10 years earlier in patients with APLA circulation compared to the general populations. APLA were detected in 65% of patients with stroke younger than 60 years and in 28% of patients with TIS [3]. APLA circulation was detected in 20% of patients with myocardial infarction younger than 45 years, with 60% consequently developing repeated thromboses. Among the multiple APLA subclasses specifically adverse effects are likely exercised by anti-β2-glycoprotein and LA phenomenon, while cardiolipin antibodies and prothrombin antibodies may play no role in development of ischemic stroke [46]. For example in recently published study by Urbanus R.T. et al. (2010), which involved 175 female patients with ischemic stroke and 203 female patients with myocardial infarction in past medical history, odds ratio for development of myocardial infarction in LA phenomenon were 5.3 (95% CI 1.4-20.8) and significantly increased with the use of OC to 21.6 (1.9-242.0) and in smoking persons (33.7 (6.0-189.0)), For ischemic stroke the similar parameters for patients with LA were 43.1 (12.2-152.0), 201.0 (22.1-1,828.0) and 87.0 (14.5-523.0). In women with anti-β2-glycoprotein the risk of ischemic stroke was increased 2.3-fold (1.4-3.7), however for myocardial infarction there were no statistically significant results [46]. Nevertheless, Cojocaru IM et al. (2007) have established the relation between increased titer of anti-cardiolipin IgG antibodies and ischemic stroke in young women [8]. Thus in order to exclude APS in patients with ischemic stroke we may recommend mandatory testing for all cofactorts of antiphospholipid antibodies [3].
Thus the role of thrombophilias in pathogenesis of gestational thromboses and significance of detected hemostasis system abnormalities for development the plan of patients’ follow-up and prevention of thromboses recurrence requires future studies.
Remote consequences and the tactics of follow-up in patients of childbearing age
Regarding arterial thrombosis, ischemic stroke is rarely a cause of maternal mortality, which can mostly be caused by secondary hemorrhage and malignant hypertension [44]. In general the lethality related to acute cerebrovascular accidents during pregnancy (4.1%) is lower than in general population in total (24%) and in people who develop stroke in young age (4.5-24%) [20]. Young patients who developed stroke during pregnancy have more reserve capacity for restoration of neurological functions. Frequently those women plan new pregnancy, which brings up for specialists the issue of follow-up of such patients and of prevention of repeated stroke during pregnancy. However there is surprisingly small number of studies that study the risk of stroke recurrence during pregnancy, pregnancy outcome in women with acute cerebrovascular accidents in anamnesis, tactics of preventive therapy, as well as the studies oriented towards development of recommendations for such patients. [9,26].
Based on some sources the possibility of stroke recurrence in repeated pregnancy is very low and amounts only to about 1%. [9,26]. С. Lamy et al. (2000) during the observation of 187 pregnancies in 125 patients suffering from ischemic stroke have registered 13 recurrences with only 2 of them being related to pregnancy. The pregnancy outcomes were similar to the ones expected for general population [26]. Due to low frequency of repeated cases of acute cerebrovascular accident the authors conclude that the stroke is not a contraindication for future pregnancies. Risk of stroke recurrence was respectively 0.5% in patients who subsequently had no pregnancies, 1.8% in patients who carried the children to full term, and differed on average by 1.3%. However the parameter was found to have a wide 95% confidence interval, due to which the real increase of risk may reach 7.5%. The study also reports the absence of strokes recurrence in 5 patients with thrombophilia during 8 pregnancies in total during which the women were given anticoagulant treatment (unfractionated heparin [UFH] or Enoxaparin). Completely different data were received from the study by Soriano D. et al. (2002), who monitored the outcome of 15 pregnancies in 12 patients with acute cerebrovascular accident in past medical history and thrombophilia (APS, deficiency of protein С, protein S, antithrombin III, MTHFR С677Т mutation). Despite the treatment with low molecular weight heparin (LMH) and aspirin during pregnancy there were detected 4 cases of thromboses recurrence (27%) and high frequency of obstetric and perinatal complications. It is worth to note that the risk of stroke recurrence in postnatal period compared to the pregnancy itself increases 2-3-fold [7,26].
Before discussing the possibility of use of different antithrombotic drugs during pregnancy we shall consider the issue of its safety for mother and for fetus. We shall immediately stipulate that the use of vitamin K antagonists during pregnancy is allowed only for women with very high risk of thromboses, namely in cases of artificial heart valves. In all other cases the compulsory transfer to UFH or LMH is needed. This requirement is caused by the fact that vitamin K antagonists permeate placenta and potentially can cause fetal growth retardation, hemorrhages in fetus and teratogenic effects [6].
The possibility of aspirin use was studied for prevention of different pregnancy complications, including the prevention of gestational toxicoses in patients from the risk group, in women with fetus loss syndrome and APS, for improvement of IVF results. The safety of aspirin use in I trimester of pregnancy is not fully clear; however there is no clear proof of unfavorable effect on fetus. Despite the fact that early retrospective studies detected teratogenic effects during use of aspirin in I trimester of pregnancy, for repeated prospective studies the results were unconfirmed. During meta-analysis of 14 randomized studies with 12,416 women who were given low doses of aspirin (50-150 mg/day) during II and III trimester of pregnancy for prevention of preeclampsia, the therapy proved to be safe for both mother and fetus [11]. Potential risk of aspirin prescription in III trimester of pregnancy includes increased risk of hemorrhagic complications in mother and in fetus, premature closing of arterial duct and (theoretically) increased duration of childbirth and tendency towards protracted pregnancy. However it is worth to note that prescription of aspirin only for prevention of thromboembolic complications is not sufficient, including the cases of patients with APS [20].
UFH and LMH do not permeate placenta and due to this do not have teratogenic effects and are not related to the risk of hemorrhagic complications in fetus. Small amounts of LMH, detected in breast milk, most likely have no clinical significance due to very low bioavailability in oral use. The complications that may arise in pregnant patient during the use of antithrombotic therapy are similar to the ones registered in general population and include hemorrhages (risk related to the use of any antithrombotic drugs), as well as heparin induced thrombocytopenia (HIT), osteoporosis and local reactions in injection sites for UFH and LMH. Risk of all the described complications in the use of LMH is much lower than in the use of UFH. The frequency of severe hemorrhages in the use of UFH during pregnancy is about 2%. Approximately 3% of non-pregnant patients receiving UFH develop HIT which may lead to the progression of existing thrombosis and to appearance of new arterial and venous thromboembolisms [48]. Based on the result of LMH use in 486 pregnant patients the frequency of slight hemorrhages was 2.7%, and no severe hemorrhages were registered [38]. Based on the data of systematic review which included 64 studies involving 2,777 pregnancy patients, frequency of severe hemorrhages in LMH use was 0.43% (95% CI 0.22-0.75%) during the pregnancy and 0.95% (0.61-1.37%) in postnatal period, frequency of wound hematomas is 0.61 (0.36-0.98), and general number of hemorrhages was 1.98 (1.5-2.57) [16]. Use of LMH during pregnancy is related to the lower risk of HIT development compared to UFH prescription and is probably even lower than in general population [16,38]. Moreover some studies show that preventive prescription of LMH during the pregnancy is accompanied by the loss of bone mass similar to the one registered for physiological pregnancy [5].
Taking into account the safety both for mother and fetus, better bioavailability, longer half-life in plasma, more predictable response to treatment and greater safety regarding development of osteoporosis and HIT, as well as greater convenience of use, LMH shall be preferred for treatment and prevention of VTE during the pregnancy.
Considering the data on relation between thrombophilia and unfavorable pregnancy outcomes, the increasing interest is paid to the use of antithrombotic therapy for prevention of not only thromboses and thromboembolisms, but also for prevention of pregnancy complications.
Based on the data of major systematic reviews the prescription of low doses of aspirin is accompanied by moderate decrease of risks of preeclampsia (approximately by 15-20%) and of other unfavorable pregnancy outcomes, including fetal and neonatal mortality, with the positive effect of antithrombotic therapy being more pronounced in women from high risk group [11]. Consequently the hypothesis was made that in women with high rigs of severe gestational toxicosis the preventive use of heparin drugs may be effective. The hypothesis is pathogenetically justified, considering that LMH possesses not only antithrombotic effects but also anti-inflammatory activity and the ability to affect placenta formation, For example, LMH was found to possess anti-apoptosis effects regarding trophoblast [18]. In the randomized study involving 80 patients with preeclampsia in anamnesis and ACE I/D gene polymorphism the prophylactic LMH prescription (Dalteparin 5,000 U/day.) was accompanied by decreased risk of preeclampsia, fetal development retardation syndrome, and improved parameters of utero-placental blood flow [30].
Combined therapy with heparin and aspirin in low doses has proven to be effective multiple times in different subgroups of patients with high risk of thrombotic and obstetric complications, including the women with venous thromboembolisms in anamnesis, patients with APS and with fetus loss syndrome [1]. Based on the data of the most recent systematic review which included 12 studies with total participation of 849 patients with APS and fetus loss syndrome in anamnesis, among all the possible interventions only UFH combined with low doses of aspirin provided reliable decrease of risk of repeated fetus loss [14]. At the same time increase of dose of UFH and aspirin was not accompanied by improvement of effect, and monotherapy with aspirin did not prove to be effective at all. Recent studies have also shown that LMH in combination with aspirin is equivalent in terms of effectiveness to UFH plus aspirin combinations.
The issue of the pregnancy follow-up in women with the stroke in anamnesis and of possibilities for prevention of repeated thrombotic complications also remains open. Based on the data of worldwide literature sources, no single protocol for such patients was developed as of yet. In opinion of a number of authors the low doses of aspirin are recommended during pregnancy and in postnatal period for patients who suffered from ischemic stroke [7,16,40,42]. Soriano D. et al. (2002) offered using low doses of aspirin in combination with prophylaxis doses of UFH or LMH in women with acute cerebrovascular accidents in anamnesis and perform thorough control of them due to high risk of both obstetric complications and the complications on part of fetus [42].
Significance of detection of genetic and acquired thrombophilia in pregnancy follow-up in patients with ischemic stroke in anamnesis
At the premises of specialized maternity clinic No.67 we examined 59 patients with strokes (average age 32±5.5 years). 22 of them had the stroke during the current pregnancy or in early postnatal period. In 20 with ischemic stroke in anamnesis (subgroup 1) we performed the planning of the present pregnancy and specific prophylaxis (low molecular weight heparin [LMH] during the entire pregnancy in postnatal period, group B vitamins, folic acid to 4 mg/day, antioxidants, aspirin based on indications), and in 17 patients (subgroup 2) the therapy was started in II - III trimester of pregnancy at the moment of address. All the patients underwent the study of hemostasis system, screening for genetic forms of thrombophilia, polymorphisms of anti-inflammatory cytokines and antiphospholipid antibodies (APLA).
Results
The main provoking factors for thromboses included the number of systemic diseases (systemic lupus erythematosis, systemic vasculitis etc.) (16.9%), oral contraceptives intake (3.4%), surgical interventions and/or traumas (1.7%), septic complications (6.8%), previously suffered thrombotic complications (27.1%), metabolic syndrome (37.3%), hypertonic disease (27.1%), heart rhythm disorder (5.1%), presence of artificial heart valves (6.8%), inadequate anticoagulant therapy in patients with mechanic heart valves (3.4%) and presence of open foramen ovale (5.1%). The multipara women (52.5%) showed significantly higher frequency of obstetric complications in anamnesis compared to the control group (69.4% respectively vs. 18.3%; odds ratio [OR] 9.6, 95% confidence interval [CI] 4.1-22.8, p<0.001), in particular fetus loss syndrome 33.3% vs 0%; p<0.001) and obstetric complications of vascular genesis (gestational toxicoses, premature detachment of a normally situated placenta, fetoplacental insufficiency, fetal growth retardation syndrome [FGRS], antenatal fetal death) (38.7% vs 11.5%; OR 10.1, 95% CI 3.8-26.5, p<0.05).
During the hemostasis system study all the patients were found to have markers of its activation: increased level of SFMC, D-dimer (on average 2-3 µg/ml with the norm to 0.5). In general the data on very burdened somatic, obstetric and family anamnesis, on development of such severe thromboembolic complications in the women of young age allowed us to hypothesize the genetic predisposition towards thromboses. Data of genetic studies were received for 51 patients. 88.2% (р<0.001 vs. 26.7% in control group; OR 20.6, 5% CI 7.4-57.5) were detected to have genetic forms of thrombophilia, with the prevalence of heterozygous FV Leiden mutation (21.6%), heterozygous prothrombin G20210A mutation (11.7%), homozygous (29.4%) and heterozygous (33.3%) MTHFR С677Т mutation, combined defects of fibrinolysis (polymorphism of genes PAI-1 4G/5G, t-PA I/D, fibrinogen -455 G/А, Hageman factor 46 С/Т) (76.5%), polymorphisms of platelet receptors genes, genes regulating renin–angiotensin–aldosterone system, as well as APLA (41.2%). In the subgroup 1 of patients where the pathogenetic therapy was started on the pregnancy planning stage the pregnancy ended in birth of live full term child in 100% of cases with the absence of severe obstetric complications. The subgroup 2 was found to have developed the severe and moderately severe obstetric complications (severe forms of gestational toxicosis, FGRS I-III, critical disorders of fetoplacental blood flow), subacute DIC-syndrome, and who frequently had the necessity of premature delivery (23.5%) and gave birth to premature hypotrophic children with low Apgar score (р<0.05 for all comparisons between subgroups 1 and 2). During the LMH therapy there was noted no development of repeated thrombotic and hemorrhagic complications.
Conclusion
Patients with acute cerebrovascular accidents in anamnesis constitute very high risk group for development of severe obstetric and repeated thrombotic complications, especially in conditions of activation of hemostasis system typical for pregnancy. Detection of multigenic forms of thrombophilia and APLA in majority of patients with acute cerebrovascular accidents allows us to establish the pathology of hemostasis as a leading cause for such complications. Thus the leading role in pathology of cryptogenic ischemic stroke in women of childbearing age is likely played by underlying hemostasis disorders, both hereditary and acquired. When planning pregnancy for the patients with ischemic stroke in anamnesis the detailed examination is required which includes the evaluation of condition of cardiovascular system, exclusion of structural abnormalities of heart, exclusion of heart rhythm disorders, as well as complex study of hemostasis system in order to detect genetic and/or acquired thrombophilias (APS, hyperhomocysteinemia). The results of such study will allow us to evaluate the risk of repeated strokes, venous thromboses and obstetric complications and to plan pathogenetically justified tactics of pregnancy follow-up. Tactics of pregnancy follow-up in women with acuter cerebrovascular accidents in anamnesis includes compulsory use of LMH during the entire pregnancy and preferably before its onset, antioxidants, group B vitamins, high doses of folic acid, antiplatelet drugs. Therapy with LMH shall be performed with control of D-dimer. Acute cerebrovascular accidents in anamnesis are the absolute indications for cesarean section. LMH shall be discontinued 24 hours before surgery and resumed 6-8 hours after it. The tactics of pregnancy follow-up developed by us using LMH under control of hemostasis system in the patients with stroke in anamnesis allowed us in 100% of cases achieve the birth of live children and avoid the development of severe obstetric and repeated thrombotic complications.
Литература/References:
1. Bates S.M., Greer I.A., Pabinger I. et al. American College of Chest Physicians. Venous thromboembolism, thrombophilia, antithrombotic therapy, and pregnancy: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines (8th Edition). Chest. 2008 Jun; 133 (6): 844-886.
2. Boekholdt S.M., Kramer M.H. Arterial thrombosis and the role of thrombophilia. Semin Thromb Hemost. 2007 Sep; 33 (6): 588-96.
3. Brey R.L. Antiphospholipid antibodies in young adults with stroke. J Thromb Thrombolysis. 2005 Oct; 20 (2): 105-12.
4. Carbillon L. Pregnancy is an essential spontaneous screening stress test for the risk of early stroke in women. Stroke. 2008 Aug; 39 (8): 138.
5. Carlin A.J., Farquharson R.G., Quenby S.M. et al. Prospective observational study of bone mineral density during pregnancy: low molecular weight heparin versus control. Hum Reprod. 2004 May; 19 (5): 1211-4.
6. Chan WS. Venous thromboembolism in pregnancy. Expert Rev Cardiovasc Ther. 2010 Dec; 8 (12): 1731-40.
7. Clark P., Greer I.A. Prevention and treatment of arterial thrombosis in pregnancy. Semin Thromb Hemost. 2003 Apr; 29 (2): 155-64.
8. Cojocaru I.M., Cojocaru M., Burcin C., Atanasiu A. Evaluation of antiphospholipid antibodies in young women with ischemic stroke. Rom J Intern Med. 2007; 45 (2): 201-4.
9. Coppage K.H., Hinton A.C., Moldenhauer J. et al. Maternal and perinatal outcome in women with a history of stroke. Amer. J. Obstet. Gynecol. 2004; 190 (5):1331-34.
10. Coppola A., Tufano A., Cerbone A.M., Di Minno G. Inherited thrombophilia: implications for prevention and treatment of venous thromboembolism. Semin Thromb Hemost. 2009 Oct; 35 (7): 683-94.
11. Coomarasamy A., Honest H., Papaioannou S. et al. Aspirin for prevention of preeclampsia in women with historical risk factors: a systematic review. Obstet Gynecol. 2003 Jun; 101 (6): 1319-32.
12. Davie C.A., OBrien P. Stroke and pregnancy. J Neurol Neurosurg Psychiatry. 2008 Mar; 79 (3): 240-5.
13. Di Carlo A., Lamassa M., Baldereschi M. et al. European BIOMED Study of Stroke Care Group. Sex differences in the clinical presentation, resource use, and 3-month outcome of acute stroke in Europe: data from a multicenter multinational hospital-based registry. Stroke. 2003 May; 34 (5): 1114-9.
14. Empson M., Lassere M., Craig J., Scott J. Prevention of recurrent miscarriage for women with antiphospholipid antibody or lupus anticoagulant. Cochrane Database Syst Rev. 2005 Apr 18; 2: CD002859.
15. Govindaiah V., Naushad S.M., Prabhakara K. et al. Association of parental hyperhomocysteinemia and C677T Methylene tetrahydrofolate reductase (MTHFR) polymorphism with recurrent pregnancy loss. Clin Biochem. 2009 Mar; 42 (4-5): 380-6.
16. Greer I.A., Nelson-Piercy C. Low-molecular-weight heparins for thromboprophylaxis and treatment of venous thromboembolism in pregnancy: a systematic review of safety and efficacy. Blood. 2005 Jul 15; 106 (2): 401-7.
17. Haywood S., Liesner R., Pindora S., Ganesan V. Thrombophilia and first arterial ischaemic stroke: a systematic review. Arch Dis Child. 2005 Apr; 90 (4): 402-5.
18. Hills F.A., Abrahams V.M., González-Timón B. et al. Heparin prevents programmed cell death in human trophoblast. Mol Hum Reprod. 2006 Apr; 12 (4): 237-43.
19. Huang T., Yuan G., Zhang Z. et al. Cardiovascular pathogenesis in hyperhomocysteinemia. Asia Pac J Clin Nutr. 2008; 17 (1): 8-16.
20. James A.H., Bushnell C.D., Jamison M.G. et al. Incidence and risk factors for stroke in pregnancy and the puerperium. Obstet Gynecol. 2005 Sep; 106 (3): 509-16. Jaigobin C., Silver F.L. Stroke and pregnancy. Stroke. 2000 Dec; 31 (12): 2948-51.
21. Kitchens K.S., Alving B.M., Kessler C.M. Consultative haemostasis and thrombosis. Elsivier Science. 2002; 617 p.
22. Kittner S.J., Stern B.J., Feeser B.R. et al. Pregnancy and the risk of stroke. N Engl J Med. 1996 Sep 12; 335 (11): 768-74.
23. Koniari I., Siminelakis S.N., Baikoussis N.G. et al. Antiphospholipid syndrome; its implication in cardiovascular diseases: a review. J Cardiothorac Surg. 2010 Nov 3; 5: 101.
24. Kupferminc M.J., Yair D., Bornstein N.M. et al. Transient focal neurological deficits during pregnancy in carriers of inherited thrombophilia. Stroke. 2000 Apr; 31 (4): 892-5.
25. Lalouschek W., Schillinger M., Hsieh K. et al. Matched case-control study on factor V Leiden and the prothrombin G20210A mutation in patients with ischemic stroke/transient ischemic attack up to the age of 60 years. Stroke. 2005 Jul; 36 (7): 1405-9.
26. Lamy C., Hamon J.B., Coste J., Mas J.L. Ischemic stroke in young women: risk of recurrence during subsequent pregnancies. French Study Group on Stroke in Pregnancy. Neurology. 2000; 55 (2): 269-74.
27. Makatsariya A.D., Bitsadze V.O., Baimuradova S.M., Dolgushina N.V., Yudaeva L.S., Khizroeva D.Kh., Akin’shina S.V. Antiphospholipid syndrome – the immune thrombophilia in obstetrics and gynecology Moscow. 2007; 456 p. [Antifosfolipidnyi sindrom – immunnaya trombofilii v akusherstve i ginekologii. M. 456 s. (In Russian)].
28. Makatsariya A.D., Beloborodova E.V., Baimuradova S.M., Bitsadze V.O. Hyperhomocysteinemia and pregnancy complications. M. 2005; 216 p. [Gipergomotsisteinemiya i oslozhneniya beremennosti. M. 2005; 216 s. (In Russian)].
29. Martinelli I., Battaglioli T., Burgo I. et al. Oral contraceptive use, thrombophilia and their interaction in young women with ischemic stroke. Haematologica. 2006 Jun; 91 (6): 844-7.
30. Mello G., Parretti E., Fatini C. et al. Low-molecular-weight heparin lowers the recurrence rate of preeclampsia and restores the physiological vascular changes in angiotensin-converting enzyme DD women. Hypertension. 2005 Jan; 45 (1): 86-91.
31. Mehdi A.A., Uthman I., Khamashta M. Antiphospholipid syndrome: pathogenesis and a window of treatment opportunities in the future. Eur J Clin Invest. 2010 May; 40 (5): 451-64.
32. Ness R.B., Markovic N., Bass D. et al. Family history of hypertension, heart disease, and stroke among women who develop hypertension in pregnancy. Obstet Gynecol. 2003 Dec; 102 (6): 1366-71.
33. Nicolaides A.N., Breddin H.K., Carpenter P. et al. European Genetics Foundation; Cardiovascular Disease Educational and Research Trust; International Union of Angiology; Mediterranean League on Thromboembolism. Thrombophilia and venous thromboembolism. International consensus statement. Guidelines according to scientific evidence. Int Angiol. 2005 Mar; 24 (1): 1-26.
34. Pezzini A., Grassi M., Iacoviello L., Del Zotto E et al. Inherited thrombophilia and stratification of ischaemic stroke risk among users of oral contraceptives. J Neurol Neurosurg Psychiatry. 2007 Mar; 78 (3): 271-6.
35. Ray J.G., Vermeulen M.J., Schull M.J., Redelmeier D.A. Cardiovascular health after maternal placental syndromes (CHAMPS): population-based retrospective cohort study. Lancet. 2005 Nov 19; 366 (9499):1797-803.
36. Roberts J.M., Cooper D.W. Pathogenesis and genetics of pre-eclampsia. Lancet. 2001 Jan 6; 357 (9249): 53-6.
37. Ros H.S., Lichtenstein P., Bellocco R. et al. Pulmonary embolism and stroke in relation to pregnancy: how can high-risk women be identified? Am J Obstet Gynecol. 2002 Feb; 186 (2): 198-203.
38. Sanson B.J., Lensing A.W., Prins M.H. et al. Safety of low-molecular-weight heparin in pregnancy: a systematic review. Thromb Haemost. 1999 May; 81 (5): 668-72.
39. Segers O., Castoldi E. Factor V Leiden and activated protein C resistance. Adv Clin Chem. 2009; 49: 121-57.
40. Sibai B.M., Coppage K.H. Diagnosis and management of women with stroke during pregnancy/postpartum. Clin Perinatol. 2004 Dec; 31 (4): 853-68.
41. Simioni P., Tormene D., Spiezia L. et al. Inherited thrombophilia and venous thromboembolism. Semin Thromb Hemost. 2006 Oct; 32 (7): 700-8.
42. Soriano D., Carp H., Seidman D.S. et al. Management and outcome of pregnancy in women with thrombophylic disorders and past cerebrovascular events. Acta Obstet Gynecol Scand. 2002 Mar; 81 (3): 204-7.
43. Szolnoki Z., Somogyvári F., Kondacs A. et al. Evaluation of the roles of the Leiden V mutation and ACE I/D polymorphism in subtypes of ischaemic stroke. J Neurol. 2001 Sep; 248 (9): 756-61.
44. Tang C.H., Wu C.S., Lee T.H. et al. Preeclampsia-eclampsia and the risk of stroke among peripartum in Taiwan. Stroke. 2009 Apr; 40 (4): 1162-8.
45. Treadwell S.D., Thanvi B., Robinson T.G. Stroke in pregnancy and the puerperium. Postgrad Med J. 2008 May; 84 (991): 238-45.
46. Urbanus R.T., Siegerink B., Roest M. et al. Antiphospholipid antibodies and risk of myocardial infarction and ischaemic stroke in young women in the RATIO study: a case-control study. Lancet Neurol. 2009 Nov; 8 (11): 998-1005.
47. Voetsch B., Damasceno B.P., Camargo E.C. et al. Inherited thrombophilia as a risk factor for the development of ischemic stroke in young adults. Thromb Haemost. 2000 Feb; 83 (2): 229-33.
48. Warkentin TE. Heparin-induced thrombocytopenia. Hematol Oncol Clin North Am. 2007 Aug; 21 (4): 589-607.
49. Witlin A.G., Mattar F., Sibai B.M. Postpartum stroke: a twenty-year experience. Am J Obstet Gynecol. 2000 Jul; 183 (1): 83-8.
50. Wiebers D.O. Ischemic cerebrovascular complications of pregnancy. Arch Neurol. 1985 Nov; 42 (11): 1106-13.
About the authors:
Makatsariya Aleksandr Davidovich – MD, corresponding member of the Russian Academy of Sciences, Professor, Head of the Department of Obstetrics and Gynecology, Faculty of Medical and Preventive, First Moscow State Medical Sechenov University. Address: ul. Zemlyanoi Val, 62-1, Moscow, Russia, 109004. Tel.: +7 (495) 788-58-40. E-mail: gemostasis@mail.ru.
Akinshina Svetlana Vladimirovna – MD, PhD, research associate of the Ob/Gyn Department of The First Moscow State Medical Sechenov University. Address: ul. Zemlyanoi Val, 62-1, Moscow, Russia, 109004. Tel.: +7 (495) 788-58-40. E-mail: svetlana_akin@mail.ru.
Bitsadze Victoria Omarovna – MD., Professor, Department of Obstetrics and Gynecology, Faculty of Medical and Preventive, First Moscow State Medical Sechenov University. Address: ul. Zemlyanoi Val, 62-1, Moscow, Russia, 109004. Tel.: +7 (495) 788-58-40. E-mail: gemostasis@mail.ru.
Zhuravleva Ekaterina Viktorovna – MD, PhD, research associate of the Ob/Gyn Department of The First Moscow State Medical Sechenov University. Address: ul. Zemlyanoi Val, 62-1, Moscow, Russia, 109004. Tel.: +7 (495) 788-58-40. E-mail: gemostasis@mail.ru.
Idrisova Larisa Emievna – PhD, researcher at the Department of the Ob/Gyn Department of The First Moscow State Medical Sechenov University Address: ul. Zemlyanoi Val, 62-1, Moscow, Russia, 109004. Tel.: +7 (495) 788-58-40. E-mail: gemostasis@mail.ru.
Abramyan Guar Razmikovna – Теl.: +37491211715. E-mail: abrahamyan.gohar@mail.ru
Сведения об авторах:
Макацария Александр Давидович – д.м.н., член-корреспондент РАН, профессор, заведующий кафедрой акушерства и гинекологии медико-профилактического факультета Первого МГМУ им. И.М. Сеченова. Адрес: ул. Земляной Вал, 62, стр. 1, Москва, Россия, 109004. Тел.: Тел.: +7 (495) 788-58-40. E-mail: gemostasis@mail.ru.
Акиньшина Светлана Владимировна – к.м.н., научный сотрудник кафедры акушерства и гинекологии медико-профилактического факультета ПГМУ И.М. Сеченова. Адрес: ул. Земляной Вал, 62, стр. 1, Москва, Россия, 109004. Тел.: +7 (495) 788-58-40. E-mail: svetlana_akin@mail.ru.
Бицадзе Виктория Омаровна – д.м.н., профессор, профессор кафедры акушерства и гинекологии медико-профилактического факультета Первого МГМУ им. И.М. Сеченова. Адрес: ул. Земляной Вал, 62, стр. 1, Москва, Россия, 109004. Тел.: +7 (495) 788-58-40. E-mail: gemostasis@mail.ru.
Журавлева Екатерина Викторовна – к.м.н., научный сотрудник кафедры акушерства и гинекологии МПФ Первого МГМУ им. И.М. Сеченова. Адрес: ул. Земляной Вал, 62, стр. 1, Москва, Россия, 109004. Тел.: +7 (495) 788-58-40. E-mail: evyashenina@list.ru.
Идрисова Лариса Эмиевна – к.м.н., научный сотрудник кафедры акушерства и гинекологии медико-профилактического факультета Первого МГМУ им. И.М. Сеченова. Адрес: ул. Земляной Вал, 62, стр. 1, Москва, Россия, 109004. Тел.: +7 (495) 788-58-40. E-mail: gemostasis@mail.ru.
Абрамян Гуар Размиковна – научный сотрудник Ереванского Научно-Исследовательского Института Акушерства, перинатологии и гинекологии, кандидат медицинских наук. Тел.: +37491211715. E-mail: abrahamyan.gohar@mail.ru
|